3.2 Population Explosion and Birth Control
In the last century an all-round development in various fields significantly improved the quality of life of the people. However, increased health facilities along with better living conditions had an explosive impact on the growth of population. The world population which was around 2 billion ( 2000 million) in 1900 rocketed to about 6 billion by 2000 and 7.2 billion in 2011. A similar trend was observed in India too. Our population which was approximately 350 million at the time of our independence reached close to the billion mark by 2000 and crossed 1.2 billion in May 2011. A rapid decline in death rate, maternal mortality rate (MMR) and infant mortality rate (IMR) as well as an increase in number of people in reproducible age are probable reasons for this. Through our Reproductive Child Health (RCH) programme, though we could bring down the population growth rate, it was only marginal. According to the 2011 census report, the population growth rate was less than 2 per cent, i.e., 20/1000/year, a rate at which our population could increase rapidly. Such an alarming growth rate could lead to an absolute scarcity of even the basic requirements, i.e., food, shelter and clothing, in spite of significant progress made in those areas. Therefore, the government was forced to take up serious measures to check this population growth rate.
The most important step to overcome this problem is to motivate smaller families by using various contraceptive methods. You might have seen advertisements in the media as well as posters/bills, etc., showing a happy couple with two children with a slogan Hum Do Hamare Do (we two, our two). Many couples, mostly the young, urban, working ones have even adopted an ‘one child norm’. Statutory raising of marriageable age of the female to 18 years and that of males to 21 years, and incentives given to couples with small families are two of the other measures taken to tackle this problem. Let us describe some of the commonly used contraceptive methods, which help prevent unwanted pregnancies.
An ideal contraceptive should be user-friendly, easily available, effective and reversible with no or least side-effects. It also should in no way interfere with the sexual drive, desire and/or the sexual act of the user. A wide range of contraceptive methods are presently available which could be broadly grouped into the following categories, namely Natural/Traditional, Barrier, IUDs, Oral contraceptives, Injectables, Implants and Surgical methods.
Natural methods work on the principle of avoiding chances of ovum and sperms meeting. Periodic abstinence is one such method in which the couples avoid or abstain from coitus from day 10 to 17 of the menstrual cycle when ovulation could be expected. As chances of fertilisation are very high during this period, it is called the fertile period. Therefore, by abstaining from coitus during this period, conception could be prevented. Withdrawal or coitus interruptus is another method in which the male partner withdraws his penis from the vagina just before ejaculation so as to avoid insemination. Lactational amenorrhea (absence of menstruation) method is based on the fact that ovulation and therefore the cycle do not occur during the period of intense lactation following parturition. Therefore, as long as the mother breast-feeds the child fully, chances of conception are almost nil. However, this method has been reported to be effective only upto a maximum period of six months following parturition. As no medicines or devices are used in these methods, side effects are almost nil. Chances of failure, though, of this method are also high.
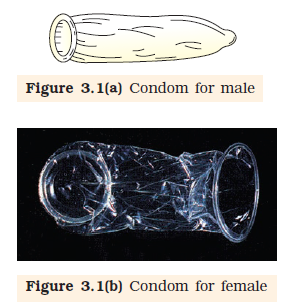
In barrier methods, ovum and sperms are prevented from physically meeting with the help of barriers. Such methods are available for both males and females. Condoms (Figure 3.1 a, b) are barriers made of thin rubber/ latex sheath that are used to cover the penis in the male or vagina and cervix in the female, just before coitus so that the ejaculated semen would not enter into the female reproductive tract. This can prevent conception. ‘Nirodh’ is a popular brand of condom for the male. Use of condoms has increased in recent years due to its additional benefit of protecting the user from contracting STIs and AIDS. Both the male and the female condoms are disposable, can be self-inserted and thereby gives privacy to the user. Diaphragms, cervical caps and vaults are also barriers made of rubber that are inserted into the female reproductive tract to cover the cervix during coitus. They prevent conception by blocking the entry of sperms through the cervix. They are reusable. Spermicidal creams, jellies and foams are usually used along with these barriers to increase their contraceptive efficiency.
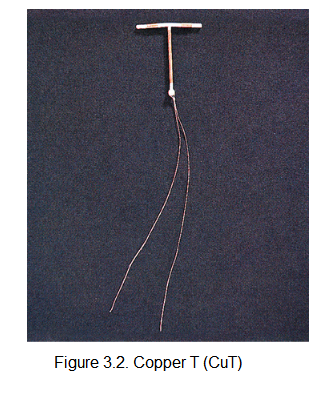
Another effective and popular method is the use of Intra Uterine Devices (IUDs). These devices are inserted by doctors or expert nurses in the uterus through vagina. These Intra Uterine Devices are presently available as the non-medicated IUDs (e.g., Lippes loop), copper releasing IUDs (CuT, Cu7, Multiload 375) and the hormone releasing IUDs (Progestasert, LNG-20) (Figure 3.2). IUDs increase phagocytosis of sperms within the uterus and the Cu ions released suppress sperm motility and the fertilising capacity of sperms. The hormone releasing IUDs, in addition, make the uterus unsuitable for implantation and the cervix hostile to the sperms. IUDs are ideal contraceptives for the females who want to delay pregnancy and/or space children. It is one of most widely accepted methods of contraception in India.
Oral administration of small doses of either progestogens or progestogen-estrogen combinations is another contraceptive method used by the females. They are used in the form of tablets and hence are popularly called the pills. Pills have to be taken daily for a period of 21 days starting preferably within the first five days of menstrual cycle. After a gap of 7 days (during which menstruation occurs) it has to be repeated in the same pattern till the female desires to prevent conception. They inhibit ovulation and implantation as well as alter the quality of cervical mucus to prevent/retard entry of sperms. Pills are very effective with lesser side effects and are well accepted by the females. Saheli-the new oral contraceptive for the females contains a non-steroidal preparation. It is a ‘once a week’ pill with very few side effects and high contraceptive value.
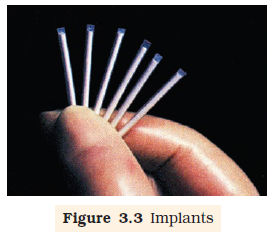
Progestogens alone or in combination with estrogen can also be used by females as injections or implants under the skin (Figure 3.3). Their mode of action is similar to that of pills and their effective periods are much longer. Administration of progestogens or progestogen-estrogen combinations or IUDs within 72 hours of coitus have been found to be very effective as emergency contraceptives as they could be used to avoid possible pregnancy due to rape or casual unprotected intercourse.
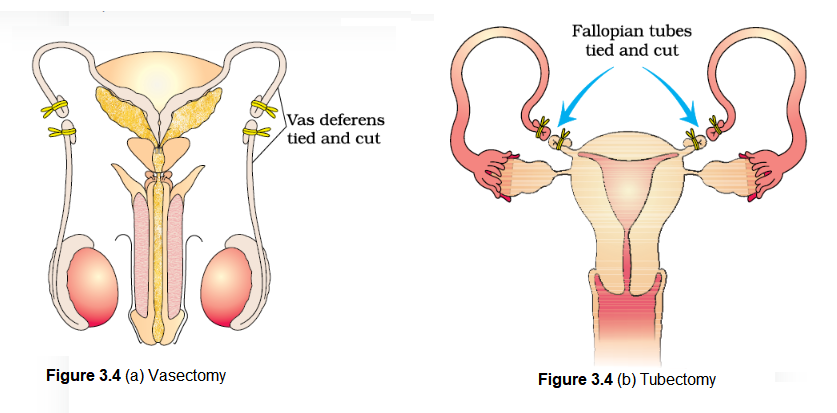
Surgical methods, also called sterilisation, are generally advised for the male/female partner as a terminal method to prevent any more pregnancies. Surgical intervention blocks gamete transport and thereby prevent conception. Sterilisation procedure in the male is called ‘vasectomy’ and that in the female, ‘tubectomy’. In vasectomy, a small part of the vas deferens is removed or tied up through a small incision on the scrotum (Figure 3.4a) whereas in tubectomy, a small part of the fallopian tube is removed (Figure 3.4b) or tied up through a small incision in the abdomen or through vagina. These techniques are highly effective but their reversibility is very poor.
It needs to be emphasised that the selection of a suitable contraceptive method and its use should always be undertaken in consultation with qualified medical professionals. One must also remember that contraceptives are not regular requirements for the maintenance of reproductive health. In fact, they are practiced against a natural reproductive event, i.e., conception/pregnancy. One is forced to use these methods either to prevent pregnancy or to delay or space pregnancy due to personal reasons. No doubt, the widespread use of these methods have a significant role in checking uncontrolled growth of population. However, their possible ill-effects like nausea, abdominal pain, breakthrough bleeding, irregular menstrual bleeding or even breast cancer, though not very significant, should not be totally ignored.
Note: The Medical Termination of Pregnancy (Amendment) Act, 2017 was enacted by the government of India with the intension of reducing the incidence of illegal abortion and consequent maternal mortality and morbidity. According to this Act, a pregnancy may be terminated on certain considered grounds within the first 12 weeks of pregnancy on the opinion of one registered medical practitioner. If the pregnancy has lasted more than 12 weeks, but fewer than 24 weeks, two registered medical practitioners must be of the opinion, formed in good faith, that the required ground exist. The grounds for such termination of pregnancies are:
- The continuation of the pregnancy would involve a risk to the life of the pregnant woman or of grave injury physical or mental health; or
- There is a substantial risk that of the child were born, it would suffer from such physical or mental abnormalities as to be seriously handicapped.